Summary
After the surgery, the pathology confirms it is Grade II Oligodendrogliomas
Arriving to Barcelona, Spain
29th of December 2020
I arrived five days prior to the surgery. The trip took around 9 hours, and I arrived safely after taking high doses of Boswellia, as per the recommendation that Michelle Gerencser gave me. The trip itself had no issues at all! (thanks to you, Michelle.)
Meeting the Neurosurgery and Doing fMRI
I met the Neurosurgery – Dr. Bartolomé Oliver, PhD. He is the head of the Neurosurgical Department at Centro Médico Teknon. He is leading nine neurosurgeons in the hospital, and he takes selected complex patients (and I was one of them). He was trained in Sweden, Switzerland, Canada, and the USA. He has 45 years of experience.
He explained in detail what to expect during the surgery and what would happen post-surgery. He also had me do another Functional MRI and blood work (a few tests) on the same day.
The blood tests had some new readings outside of the readings, and I could not know the reason this took place (the tests are Complete blood count, VSG, Platelets, Blood glucose, total bilirubin, Creatinine, Urea, GOT and GPT, Alkaline phosphatases, and Electrolyte Panel). You can download the blood tests here. (I wonder if these readings showed up differently because of what I did few weeks before traveling, as I was on the Ketogenic Diet, and I took 12 HBOT sessions right before surgery)
The Functional MRI took place in another hospital because he said that the best ones were there. Once I arrived there, I found that Dr. Bartolome was there too. Dr. Pujol and Dr. Deus worked on my case for the fMRI . One of the doctors has 28 years of experience, and he said he was the first doctor to work on fMRIs in all of Europe. He explained to me the outcome, explaining that one part that has the largest tumor area is safe to cut off, but the area that is related to words and memory is not safe to cut off. Below are the key images from the fMRI
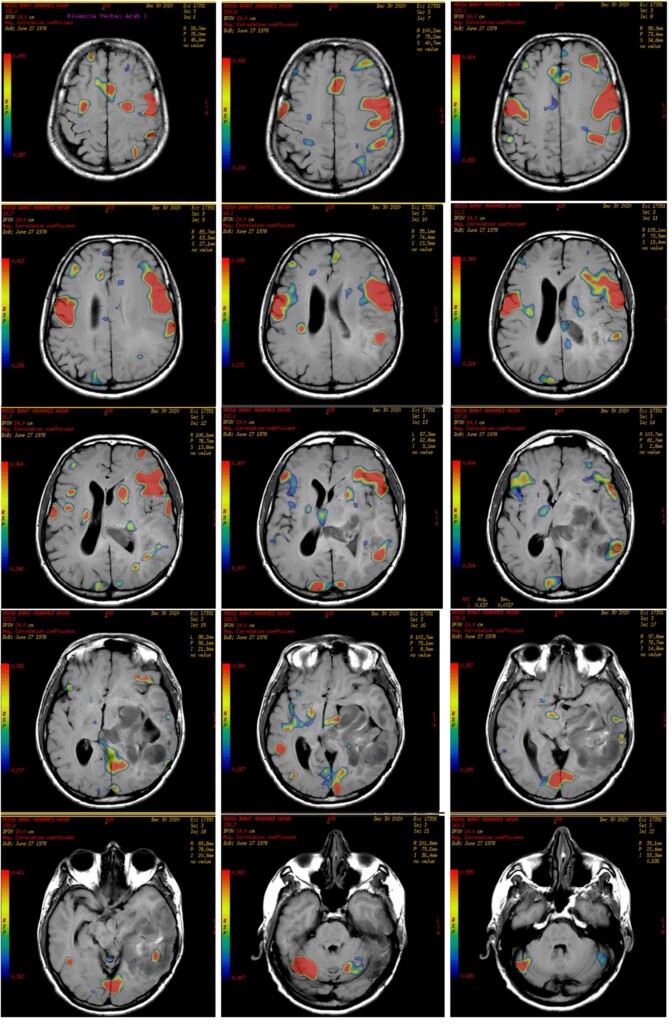
Dr. Bartolomé stated again that 70% of the brain tumor area will be removed, while the other most likely won’t be touched.
It is important to know that I have communicated with three fine neurosurgeries in the United States and one in Amman, Jordan, and all of them looked at the MRIs, and they all said that only 70% of the surgery is possible (and that the surgery is recommended and must take place immediately). They all said that the new tumor is going to be either Stage 3, Stage 4, or a combination of both.
Pre-Operative Coagulation Assessments and Tests
One of the doctors took around an hour of assessments (questions, games, photos-to-names, etc.). She stated that there are areas above average and others below average. The ones I was challenged with were finding words for selected photos and remembering the photos if I was asked after a few minutes.
The plan is that parts of these tests will be done again just before surgery and during the surgery when I am awake to compare my situation to how it would behave on the targeted resection during this surgery.
I had asked them to take videos and photos, and they were kind enough to share them.
January 4th, 2021: The Surgery
I was at the hospital at 9 a.m. and was bored for a few hours.
At 2:00 PM, I took a specific shower to clean my head before surgery. At 2:30 PM, I said good-bye to my wife and went for surgery.
First, I had an X-ray, and that showed that everything was alright. Then, around 3:00 PM, I was in the surgery room (looking nice and comfortable).
The surgery itself took place at 3:30 PM and finished at 10:30 PM (8 hours)
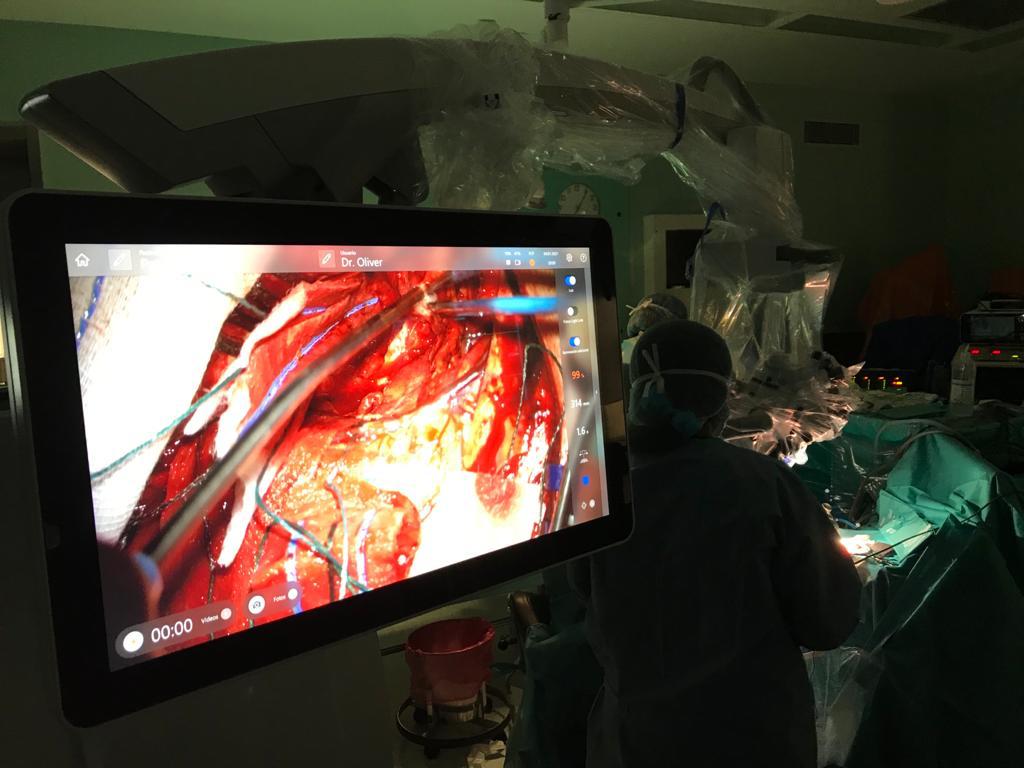
Photos and videos took place during the surgery. That was kind of Dr. Bartolomé, as per my request when I saw him on the first day.
Tools and Techniques During Surgery
Dr. Bartolomé said that during the surgery, the following will take place:
- Awake craniotomy
- Neurophysiological and Neuropsychological intraoperative monitoring
- Neuronavegation
- Ultrasonic aspirator (CUSA)
- Kinevo for fluorescein guided resection – GLIOLAN (5-ALA) protocol
The doctor used fluorescence-guided imaging to clearly see the high-grade (stage 2 and stage 4) cells to ensure resection of the right temporal areas. You can watch this video in which another doctor shares how the high grade is much easier to see during surgery.
Surgery Room
I met all the doctors, and they explained the process to me. They put me in a comfortable setting and put many devices on the back, on the head, and other places. After they made sure that I was in a comfortable set-up and location, I was given something to sleep in. I started reading at 10. Even though I wanted to count to 20, I slept after counting only :)
Opening the Brain
I was told that it will take an hour after my brain is clean and ready to be worked through. They took it in 45 minutes (15 minutes less). How come? Well, the doctor said that obviously, the surgery in 2009 was not closed properly. Dr. Oliver said that they were surprised given that it’s weakly open outside. Lucky for me, I have had no hits on the brain since then!
The surgery took place at 3:30 PM and finished at 10:30 PM (around 8 hours)
Awake Craniotomy
When they woke me up, I told them several times that I was sleepy and wanted to sleep (I don’t remember that). The doctor was patient and gave me 15 minutes to wake up.

I do remember the first two minutes, where they started asking me the targeted questionnaires. The Neuropsychologist did the operative coagulation assessments in English and had a colleague who did them in Arabic too. The team told me that I actually did a better job than the time they did it an hour before surgery. That’s why the doctor decided to resect the area without waking me up again (it was planned to be done twice).
Fluorescein-Guided Resection
The photos below show that during the resection, the doctor did not find any tumors in the colors that the GLIOLAN was to show. The doctor did not share that fact with me post-surgery and wanted to see what the purpose was that neither Stage 3 nor Stage 4 tumors showed up. He wanted to wait until the Pathology showed.
Tumor Resection Work!
The videos show parts of areas that they cut off, and these are 4 videos, where each of them is less than 5 minutes each. You can see them here if you feel comfortable watching those videos.
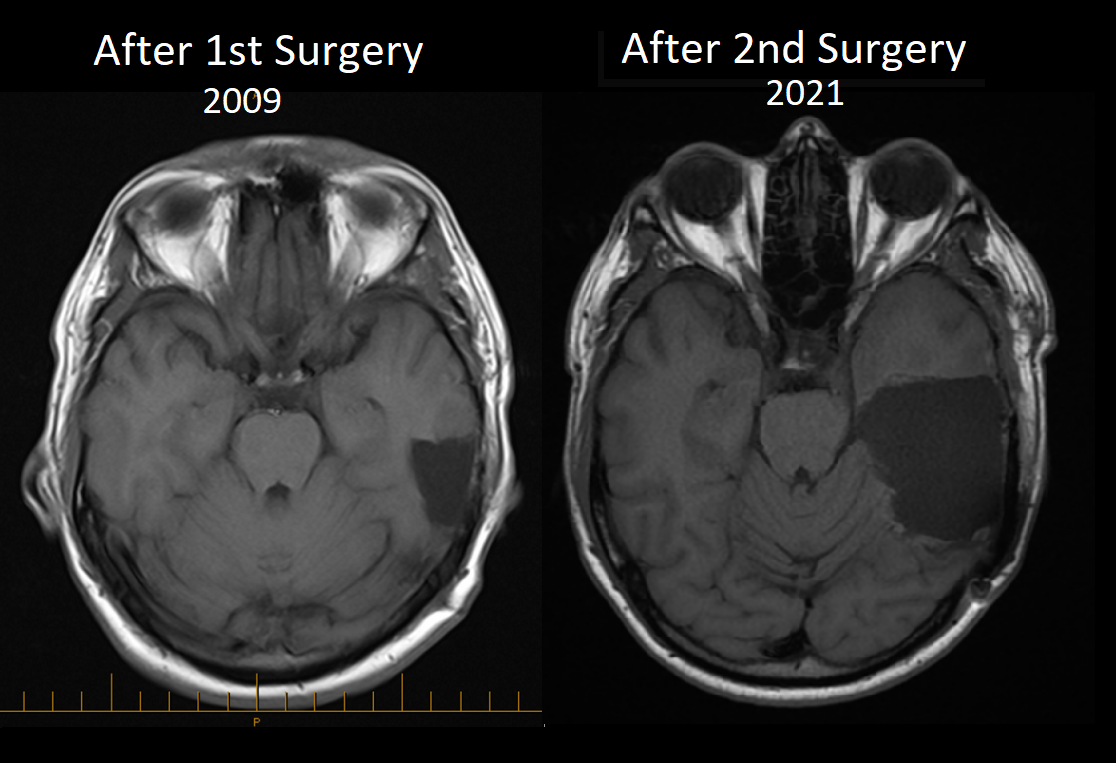
Compare!
I decided to compare the images of the first brain tumor resection with the newer one.
Clearly, the amount that was cut is significantly larger.