How Many So Far?
I’ve taken probably 39 MRI scans since 2006. Almost all of these tests were contrasted until I discovered that making so many MRI scans with gadolinium-based contrast was a bad decision. Therefore, in early 2018, I began to omit part of the contrast with each MRI until I was told that development had taken place and I started taking contrast (starting in December 2020).
Most Recent MRIs
December 10th, 2023
You can download the MRI immediately online by clicking here.
The report is not yet out. The device used was Closed MRI with 1.5 tesla GE American
Sept 7th, 2023
You can see the MRI immediately online by clicking here.
The latest report below mentions that it has some cancer growth
Axial Flair, T1, DWI and T2 weighted images; sagittal T2 and coronal T2 weighted images were obtained. Thin slices Cube T2 FLAIR images were also obtained.
- The irregular-shaped lesion within left temporal lobe appears larger in current study as compared to previous study dated 7.1.2023
- The thickness of medial aspect of the posterior part of the lesion within the left temporal lobe measures 17.8mm in current study and 15.4mm in old study.
- Medial to lateral width of the medial part of the lesion of left temporal lobe close to sella turcica is 23.9mm in the current study whereas it measures 22.8mm in old study.
- The midline shift of the lesion measures about 7.5mm just posterior to the left thalamus whereas it measures 6.8mm in old study.
Jan 5, 2023
You can see the MRI immediately online by clicking here
This was exactly 2 years post my previous surgery. The report said the following:
The previously visualized mass lesion in left cerebral hemisphere appears almost the same as in previous study with no significant changes seen regarding size, signal intensity, extension of this mass lesion and the white matter edema.Axial Flair, T1, DWI and T2 weighted images; sagittal T2 and coronal T2 weighted images were obtained.
A comparison with previous MRIs dated 14.6.2022 and 21.9.2022 has been done.
No appreciable enhancement could be seen as well
Sep 21, 2022
The report said the following:
Axial Flair, T1, DWI and T2 weighted images; sagittal T2 and coronal T2 weighted images were obtained.
Comparison with previous MRIs dated 14.6.2022 and 2.1.2022 has been done.
-
- The previously visualized mass lesion in left cerebral hemisphere appears almost the same as in previous study with no significant changes seen regarding size, signal intensity and extension of this mass lesion.
More MRIs can be shared with you upon request
June 14, 2022
Axial Flair, T1, DWI and T2 weighted images; sagittal T2 and coronal T2 weighted images were obtained.
Comparison with previous MRI dated 2.1.2022 has been done.
-
- The previously visualized mass lesion in left cerebral hemisphere appears almost the same as in previous study with no significant changes seen regarding size, signal intensity and extension of this mass lesion.
More MRIs can be shared with you upon request
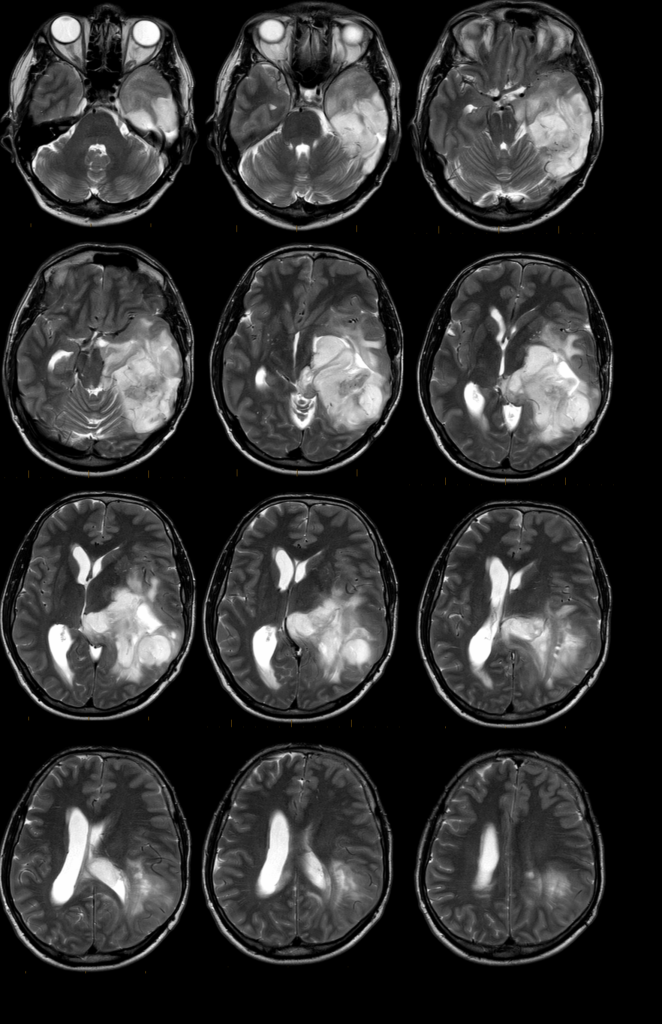
June 14, 2021
Flair, T1, DWI and T2 weighted axial with T2 sagittal and coronal images were obtained. postcontrast T1wi were obtained. Comparison with previous MRI images dated 4 Feb 2021 has been done. Previous MRI was done without IV contrast.
-
- Evidence of previous craniotomy with partial tumor resection referring to MRI images prior to previous study. • Dimensions of residual tumor within left lateral ventricle in current study are 28x28x16 mm which is smaller than previously seen.
-
- The left middle cranial fossa CSF intensity fluid appears slightly more pronounced than in previous study now measuring 58x46x31mm.
-
- Extensive white matter edema is noted within left temporal and occipital lobes in current study which appears almost the same as in previous study.
-
- The previously visualized hemorrhagic areas within left temporal lobe are no longer seen and have mostly resolved.
-
- No appreciable enhancement could be seen following IV contrast administration.
-
- No significant shifting of midline structures could be seen.
-
- No other significant changes could be seen compared to previous study.
-
- The documented focal bulge superior to left zygomatic arch is probably attributed to a metallic implant in the region that grossly measures 19mm long.
More MRIs can be shared with you upon request
Feb 5, 2021
So that took place right after the surgery
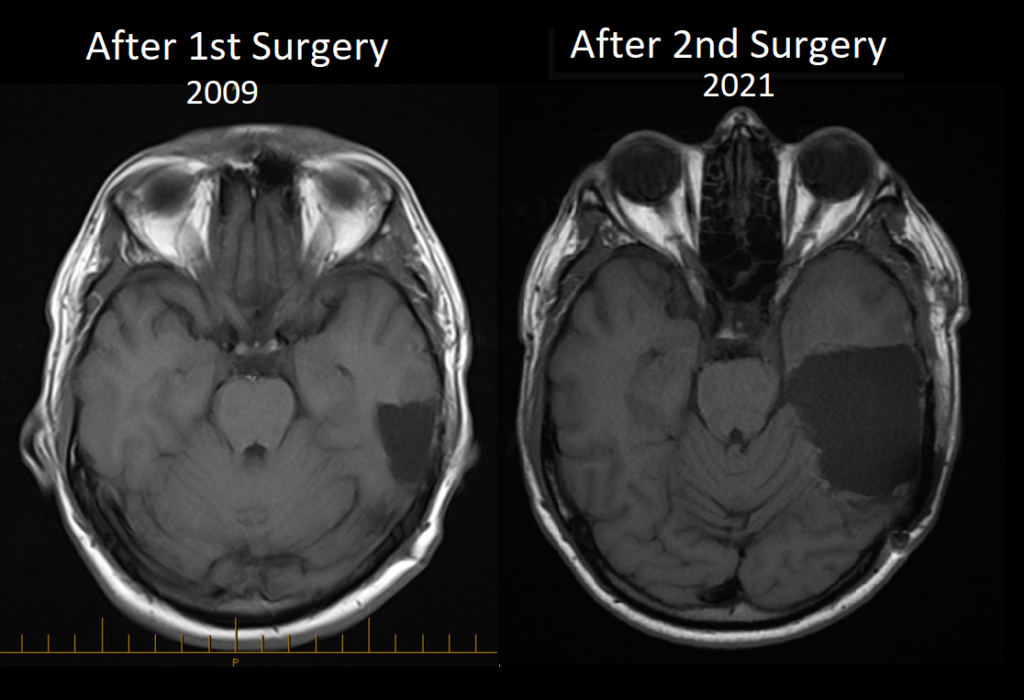
Below is a better view view that shows what actually remained untouched after the surgery
The Neurosurgeon, Dr. Oliver stated that he can remove further of these remaining with another surgery after 3 to 6 months of the first surgery, but he stated that this is not an “emergency” and that it can wait.
This MRI which took place on February 4th, can be downloaded here, and you can also have a quick look in YouTube below
The report that came from the Radiologist is different than the one in Spain (right after the surgery). You can download the one-day report by clicking here.
This report pushed me to meet with Dr. Oliver again, and that took place, and the details of that meeting can be seen here.
Jan 5, 2021
You can also have a look at the MRI that took place one day after the surgery, on January 5, 2021. You can also download that here
Before the Second Surgery
December 30th, 2022
Spain
On December 30th, a few days before the second surgery, Dr. Oliver asked for an MRI and fMRI prior to the surgery. As you’ll see later, I did this a few weeks before in King Hussien, but he did not feel confident that the fMRI was done best.
You can download the MRI/fMRI by asking me to share it with you (I did not publish because it’s large, around 600 MB)
Before Leaving to Spain
I did an MRI on December 2nd, 2020, with contrast and Functional MRI. It was done at The King Hussein Cancer, and three reports showed information as follows:
I made a short video from the outcome of this MRI with Contrast
This MRI with Contrast, along with the Functional MRI is big (~500MB) and can be downloaded and reviewed for whoever is interested.
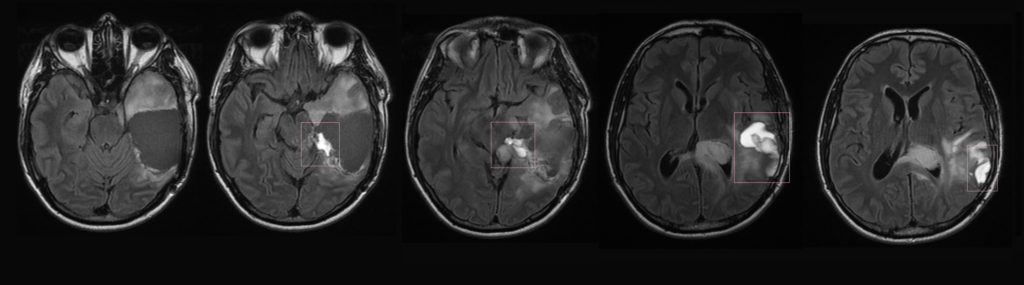
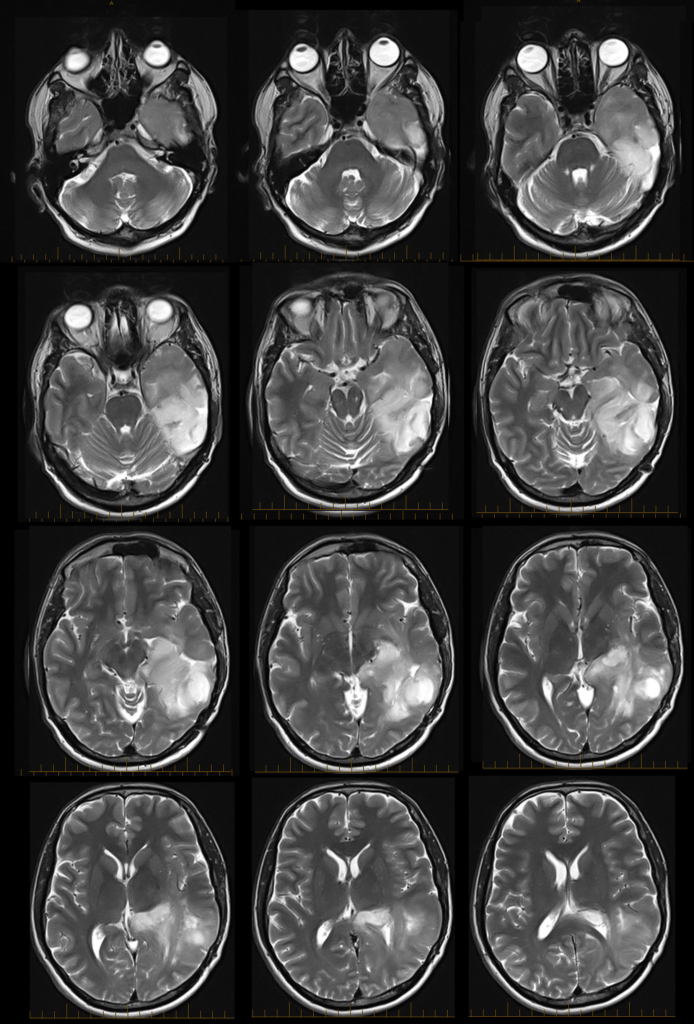
Compare Important Images
I chose to help you see what things looked like against different years.
The first 12 photos below are the most recent one. The others are 2018 and 2012. The growth in 2018 (and 2019) was not seen as real growth, per Dr. Richard Cooper. Therefore, I did not take action. However, the brain neurosurgeon believes I’m late and should be taking surgery immediately. He believes he will safely remove it all and that only one area won’t be resected in the middle of the brain.
Quick MRI Reading?
Don’t want to download large files and yet want to see the MRI quickly from your browser? (These are for the last five MRI scans only)
To sign in, you’ll go to
https://cloud82.carestream.com/portal/WebLogin.aspx
For the password, please write to me through the contact me page so I can share the password with you immediately!
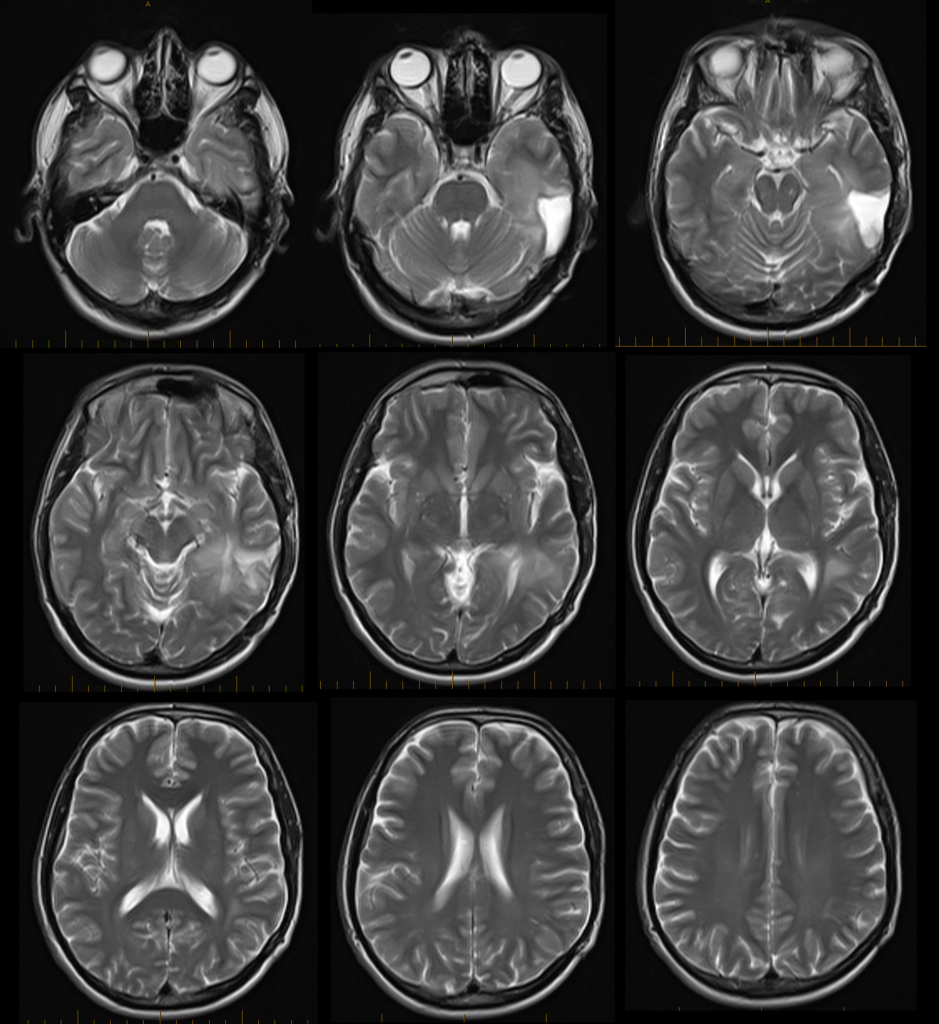
In the meanwhile, the below are the Reports on the last few MRIs
Quick Brief About Reports
November 2nd: Most Recent MRI
Here is the report outcome:
Limited examination as no IV contrast were administered
Evidence of huge, lobulated, heterogenous abnormal signal intensity was seen in the left temporoparietal lobe, which shows no significant changes in bulk or signal characteristics when compared with the previous study dated July 12, 2020.
Previously seen areas of low and high signal intensities, which may represent blood, show no significant changes in the current study.
The midline shifts to the right side, almost unchanged, which also includes the mass effect on the left pons and left brain stem.
The effacement of ventricles are almost the same as previous examination.
In the current study, there is hypertrophy of left nasal turbinates and mucosal thickening of left ethmoidal air cells, previously were more on the right side.
Nasal septum deviation as well as the polypoid and mucosal thickening, which may represent retention cyst versus small polyp measuring 1 cm in diameter involving the left maxillary antrum, seen unchanged
This outcome made me feel that my brain cancer is developing slowly, and I am deciding to do something about it. Initially, I will listen to what King Hussein Cancer Center (KHCC) will say, switch to Ketogenic Diet, and will go back to doing HBOT. Reaching KHCC will surely require repeating MRI, and will surely ask for Contrast.
I felt better about taking a Contrast after I had done
July 12th, 2019
This MRI test was conducted a day before I started my HBOT sessions.
The outcome was shared as per the below (which made me feel safe to forward with HBOT)
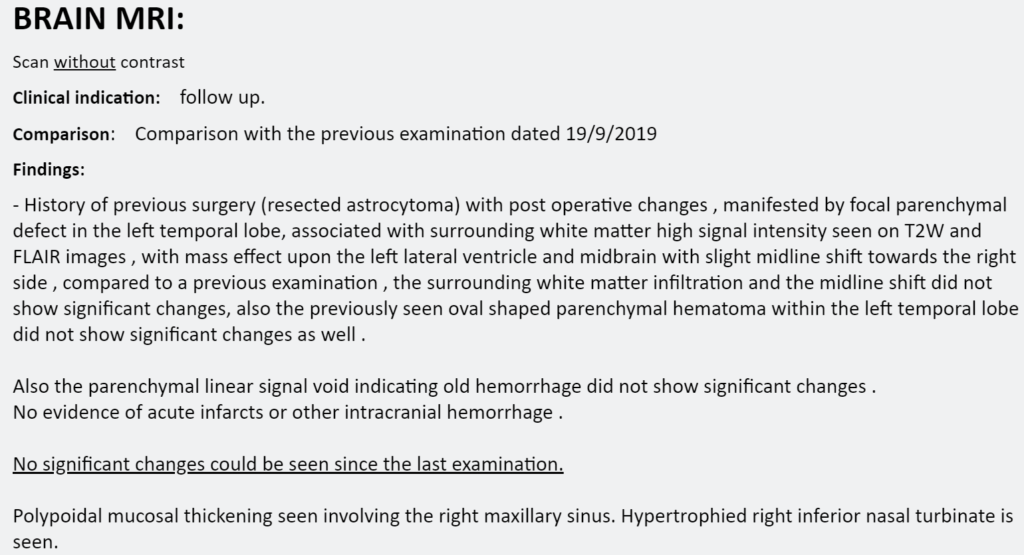
Sep 19th, 2019
Just before traveling to the states and going for a SPECT, I decided to make yet one more MRI.
The outcome was as per the below
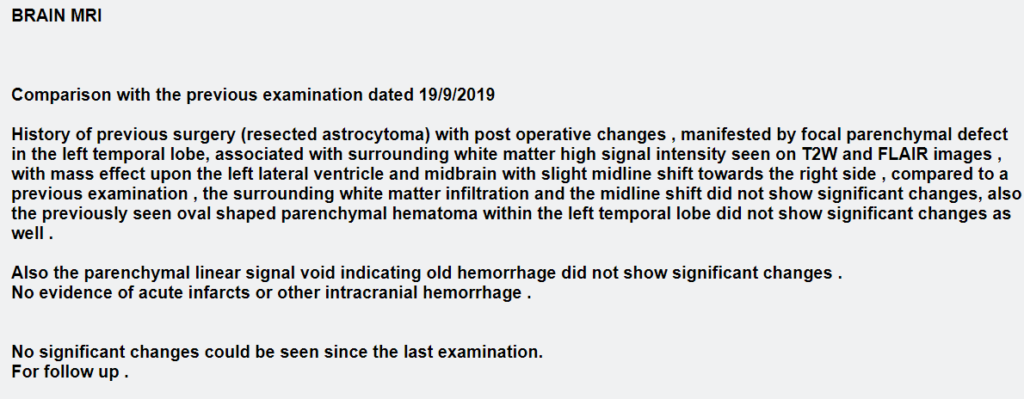
This test was one month after starting to go through ketosis as I started on Ketogenic diet.
I will be seeking the opinion of Dr. Richard Cooper to hear what he has to say.
You can see the MRI itself by going to the area called “Quick MRI Comparison” below.
July 2019, Right Before Above
This MRI was somewhat different in comparison to the recent ones, and therefore I asked Dr. Richard Cooper for his professional review.
Here are his thoughts:
The MRI findings and the MRS peaks observed on the MRI that I wrote you about before are more consistent with benign gliosis than a recurrence or the interval development of tumor cells.
The glial cells are basically the group of ’support cells’ that provide protection, nourishment, and other forms of support for the neurons in the brain. They are typically interspersed throughout the neurons, and they are responsible for the myelination process that covers the nerve cells with the fatty coating they need to transmit signals along pathways.
Gliosis is basically somewhat of a generic term for the dysfunction and changes that develop in these cells after any kind of trauma or an infection. In this case, the surgery was the traumatic event, and post-surgical gliosis is a very well known and common phenomena. It tends to have particular MRI traits and maintain a stable appearance over time. The MRI features match the findings on the most recent MRI.
Gliosis is one of the false-positive causes for MRS values that correspond to the high and low values seen when tumor cells are present — basically the injured glial cells and the tumor cells are both ‘leaky’ and thus have similar traits and MRS values.
There is a lot more to dive into regarding gliosis and what kinds of things we might try to decrease it or overcome it, but it is a natural part of the brains response to injury and it does not typically cause problems or affect function or behavior.
The main thing is that it is benign, natural, and present – therefore it explains the observed MRS findings. In addition, there are no secondary findings present to suggest developing tumor cells — no new areas or enlarged regions or mass effect/midline shift or other changes to suggest that a process of growing cells has started. This is probably why the reader of the exam made the addendum that he did where he explains the findings but then just basically says “possible neoplasm, for follow-up” instead of coming down hard about tumor cells or suggesting further evaluation or neurosurgical consult.
Dr. Richard Cooper, Fri Aug, 2nd 2019
In comparison to the one in Jan 2019 (4 months before), it is clear that there is something slightly different.
Full List of Brain MRI Reports
All MRI reports have been saved. Some were taken for a second opinion. 31 reports can be downloaded here.
Historical Brain MRI Scans
All MRI scan files, from before my surgery in 2006 until now, can be downloaded upon request.
Functional MRI Documents
I have access to like two fMRI, and MRS. One took place in 2009, and the other was one day before the second brain surgery that took place in January 2021. You can download the entire fMRI here (220 mb)
