I first met Dr. Richard in 2018. He drove several hours across the states to see me at another doctor’s office to help me with my case. I have yet to meet a doctor who is that giving, that dedicated, and that caring for his patients.
The second time I met at the NeuroRadiance office in Ohio, where we worked on giving me Laser therapy transcranial Near-Infrared Laser Application and he chose to give it to me in places away from where my cancer was/is. I took 6 sessions, and I remember that what he did gave me my dreams back for a few weeks!
Aside from that part, I do not depend on him except on reading my MRIs because he pays far more attention than others I worked with in the past in that area!
SPECT Scan Analysis
The doctor gave me his time to look at my SPECT Scan that took place in September 2019. Here are his thoughts as I got them:
- CONGRATULATIONS!!
The SPECT definitely proves that you do not have residual tumor cells in your brain – the surgical region showed no little spikes or areas of increased flow and no patterns that would suggest tumor growth of any kind. This is confirmed with the stability on the MRI images, but until the SPECT it was possible that some cells were still present that could become a problem.
Now you can consider yourself cured of grade II astrocytoma despite all the things we think and hear about those kinds of tumors!! This is a tribute to all that you have done.
I wasn’t sure if they pointed this out or not, but the absence of activity in the region of the surgery is significant — and remember you have neuroplasticity on your side and the lack of blood flow activity in this region does not mean a lack of function — pathways have changed and rerouted and function can remain intact. - I wasn’t sure if they explained the observation regarding the area of decreased flow being larger than the surgical bed itself.
This is expected and OK and relates to tumor growth and surgical principles.
In stroke patients, we think of it sort of like a target sign in which a small central area of terminated neurons is surrounded by a larger region of brain tissue that is stunned from getting less than normal oxygen and nutrients for an extended time frame (they get enough to survive but not enough to keep from being injured).
The larger area is called the ‘ischemic penumbra’ and the care of stroke patients revolves around trying to save and revive as much of this region as possible.
The mechanism for a brain tumor and the surgery is a little bit different but the result is the same – the area surrounding the surgical bed and the involved hemisphere of the brain are the areas we are trying to improve – not so much the surgical bed itself.
In your case this area showed reduced activity relative to normal but more activity through the whole region than is normally seen after that type of surgery. So I don’t think of it as a negative. Typically, the SPECT defect after that surgery is often more than double the size of the tumor itself - The color changes in the non-surgical regions are why he asked you about accidents or other injuries besides the surgery itself, and I hadn’t previously realized that you had been in an MVA years ago. Those kinds of things add up on a person and create cumulative changes.
When that happens, the SPECT colors establish that you are functioning at your current level without having complete access to your brain’s abilities and potential – thus in some cases it goes unnoticed while in other cases methods to improve blood flow and activity in these areas leads to clearly recognizable changes that enhance the person’s quality of life.
It falls more within the spectrum of self-awareness, adaptability and the desire for ongoing forward progress than it is a statement about the person’s brain function and ability. In other words, it is changeable and not a prognostic indication that there is only so far you can go before hitting a permanent plateau.
MRI: Sep 19th, 2019
Just before traveling to the states, and going for SPECT, I decided to have yet one more MRI.
I have not yet hear from Dr. Richard, and until he does…. here is what the official MRI report said
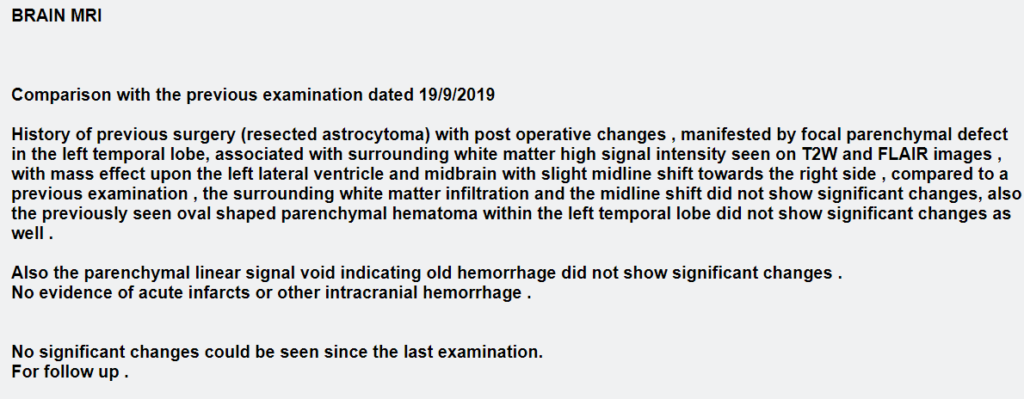
This test was one month after having started the Ketogenic diet.
You can see the MRI itself by going to the area called “Quick MRI Comparison” here.
MRI: July 2019
This MRI was somewhat different in comparison to the recent ones, and therefore I asked Dr. Richard Cooper for his professional review.
Here are his thoughts:
The MRI findings and the MRS peaks observed on the MRI that I wrote you about before are more consistent with benign gliosis than a recurrence or the interval development of tumor cells.
The glial cells are basically the group of ’support cells’ that provide protection, nourishment, and other forms of support for the neurons in the brain. They are typically interspersed throughout the neurons, and they are responsible for the myelination process that covers the nerve cells with the fatty coating they need to transmit signals along pathways.
Gliosis is basically somewhat of a generic term for the dysfunction and changes that develop in these cells after any kind of trauma or an infection. In this case, the surgery was the traumatic event, and post-surgical gliosis is a very well-known and common phenomena. It tends to have particular MRI traits and maintain a stable appearance over time. The MRI features match the findings on the most recent MRI.
Gliosis is one of the false-positive causes for MRS values that correspond to the high and low values seen when tumor cells are present — basically the injured glial cells and the tumor cells are both ‘leaky’ and thus have similar traits and MRS values.
There is a lot more to dive into regarding gliosis and what kinds of things we might try to decrease it or overcome it, but it is a natural part of the brain’s response to injury, and it does not typically cause problems or affect function or behavior.
The main thing is that it is benign, natural, and present – therefore it explains the observed MRS findings. In addition, there are no secondary findings present to suggest developing tumor cells — no new areas or enlarged regions or mass effect/midline shift or other changes to suggest that a process of growing cells has started. This is probably why the reader of the exam made the addendum that he did where he explains the findings but then just basically says “possible neoplasm, for follow-up” instead of coming down hard about tumor cells or suggesting further evaluation or neurosurgical consult.
Dr. Richard Cooper, Fri Aug 2nd 2019
